Basel, Switzerland (UroToday.com) Dr. Mack Roach presented on radiotherapy options for patients with clinical node-positive prostate cancer.
The talk began with trying to define the optimal candidate for salvage lymph node dissection (SLND) for nodal recurrence of prostate cancer. Fossati et al.1 published a study that included 654 patients who experienced prostate-specific antigen (PSA) rise and nodal recurrence after radical prostatectomy and underwent SLND at nine tertiary referral centers. Lymph node recurrence was documented by PET/CT scan using either 11C-choline or 68Ga-labeled prostate-specific membrane antigen ligand. The median follow-up was 30 months among patients without clinical recurrence, and 334 patients developed clinical recurrence after SLND. The Kaplan-Meier curve demonstrated that the probability of early clinical recurrence was 25%. Multivariable analysis showed that Gleason grade group 5 (hazard ratio [HR]: 2.04; p<0.0001), time from radical prostatectomy to PSA rising (HR: 0.99; p=0.025), hormonal therapy administration at PSA rising after surgery (HR: 1.47; p=0.0005), retroperitoneal uptake at PET/CT scan (HR: 1.24; p=0.038), three or more positive spots at PET/CT scan (HR: 1.26; p=0.019), and PSA level at SLND (HR: 1.05; p<0.0001) were all significant predictors of clinical recurrence after SLND.
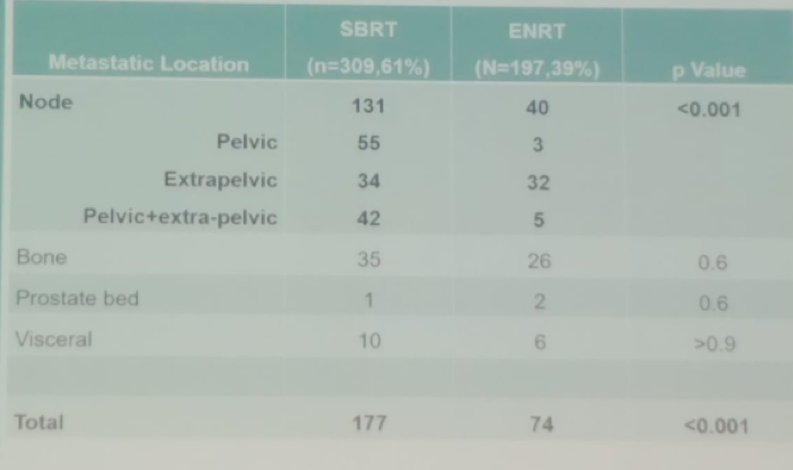
Another mentioned study was a multicenter retrospective study that assessed metastases directed therapy in the form of radiotherapy, in treating nodal oligorecurrent prostate cancer patients (five or fewer lymph nodes). The study compared stereotactic body radiotherapy (SBRT) to elective nodal radiotherapy (ENRT)2. The primary endpoint of the study was metastases free survival (MFS). ENRT was associated with fewer nodal recurrences compared with SBRT (p < 0.001). In a multivariable analysis, patients with one lymph node at recurrence had longer MFS after ENRT (hazard ratio: 0.50, 95% confidence interval 0.30-0.85, p = 0.009) (Figure 1). Late toxicity was higher after ENRT compared with that after SBRT (16% vs. 5%, p < 0.01). The modified pattern of progression following SBRT or ENRT is shown in Table 1. Dr. Roach emphasized that this study showed that patients with a single positive node benefited more with ENRT than with SBRT.
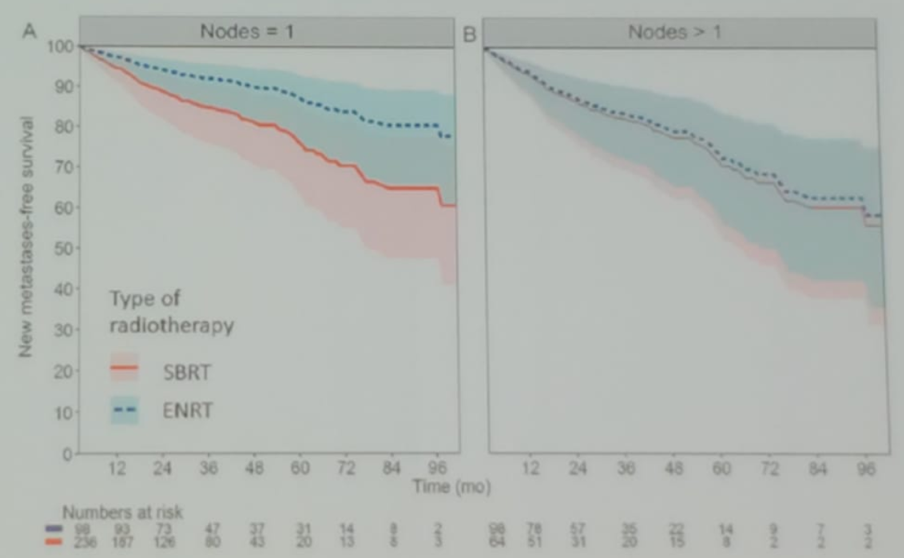
Figure 1. Difference in adjusted metastases free survival following SBRT vs. ENRT in patients who were treated with radical prostatectomy at diagnosis and presenting with N1 recurrence and no treatment with androgen deprivation therapy (ADT), with a PSA less than 4 ng/ml at recurrence.
Table 1. Modified pattern of progression in SBRT vs. ENRT
There is also debate around the template of primary lymphatic landing sites of the prostate and which template should be used for radiotherapy. Different studies have shown various templates, and a multimodality mapping study by Mattei3 demonstrated that PLND for prostate cancer should include the external and obturator regions, as well as the portions medial and lateral to the internal iliac vessels, and the common iliac lymph nodes at least up to the ureteric crossing. This extended lymph node dissection should be done to achieve a removal of approximately 75% of all nodes potentially harboring metastasis (Figure 2).
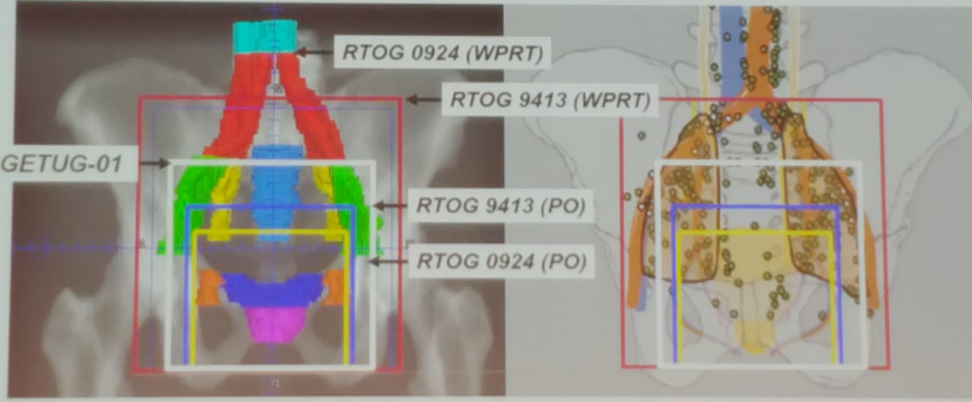
Figure 2. Various PLND templates in prostate cancer
Next, Dr. Roach discussed the role of adding ADT to radiotherapy. In 2006 it was shown that the addition of ADT to radiotherapy in the treatment of patients with lymph-node positive disease conferred a significant overall survival advantage (Figure 3)4. There have been two phase III trials comparing ADT + radiotherapy to radiotherapy alone in lymph-node positive disease. Both studies demonstrated improved survival with the addition of ADT (Figure 4).
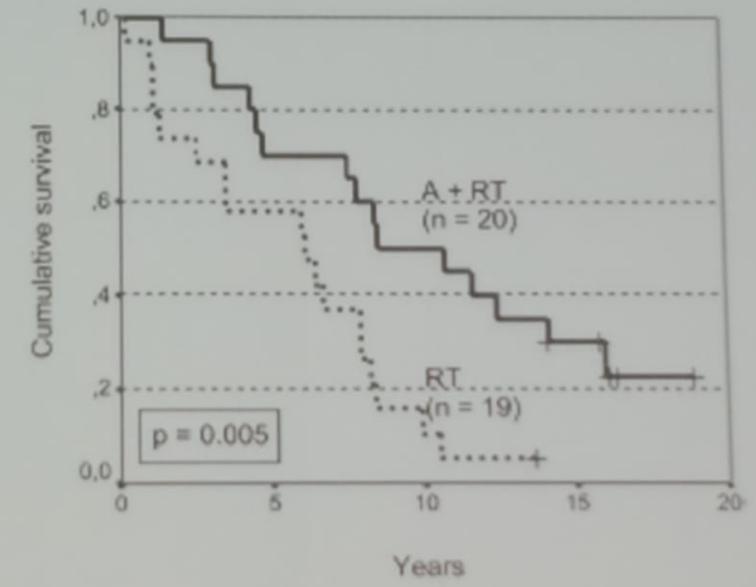
Figure 3. Kaplan Meier curve comparing overall survival of patients with and without ADT combined with radiotherapy for lymph-node positive disease
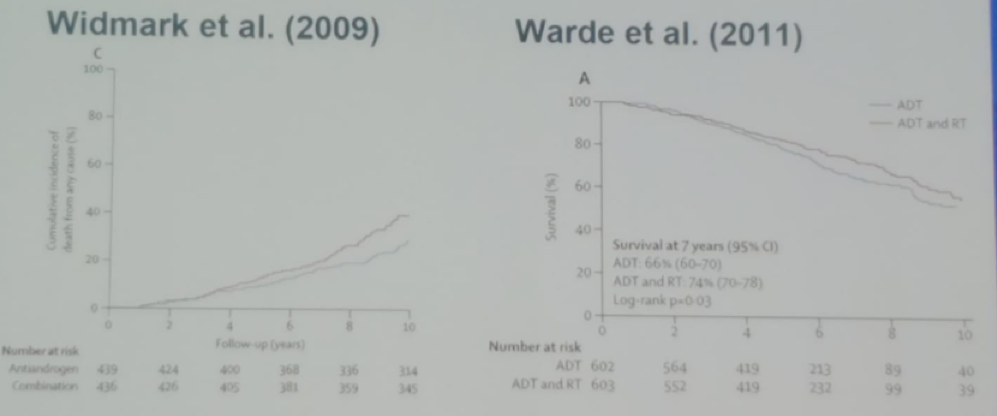
Figure 4. Two additional trials showing a survival benefit with the addition of ADT to radiotherapy in lymph-node positive disease
The NRG/RTOG 9413 study showed that whole pelvic radiotherapy (WPRT) plus neoadjuvant hormonal therapy (NHT) improved progression-free survival in patients with intermediate-risk or high-risk localized prostate cancer compared with prostate only radiotherapy plus NHT, WPRT plus adjuvant hormonal therapy (AHT), and prostate only radiotherapy plus AHT. In the long-term update after 10 years of follow-up, the results remained the same, showing that WPRT + NHT improved progression-free survival compared with NHT plus prostate only radiotherapy and WPRT plus AHT, despite the increased risk of grade 3 or worse intestinal toxicity. Interestingly, the interactions between radiotherapy and hormonal therapy suggested that WPRT should be avoided without concomitant NHT5.
Dr. Roach concluded his interesting talk and stated that there are still many unanswered questions for the use of WPRT which include the use of small field vs. large field, potential morbidity, and cost.
Presented by: Mack Roach III, MD, Professor of Radiation Oncology and Urology, Department of Radiation Oncology, University of California San Francisco
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New-York, USA, Twitter: @GoldbergHanan at the 2019 Advanced Prostate Cancer Consensus Conference (APCCC) #APCCC19, Aug 29 – 31, 2019 in Basel, Switzerland
References:
1. Fossati, Nicola, Nazareno Suardi, Giorgio Gandaglia, Carlo A. Bravi, Matteo Soligo, R. Jeffrey Karnes, Shahrokh Shariat et al. “Identifying the optimal candidate for salvage lymph node dissection for nodal recurrence of prostate cancer: results from a large, multi-institutional analysis.” European urology75, no. 1 (2019): 176-183.
2. De Bleser, Elise, Barbara Alicja Jereczek-Fossa, David Pasquier, Thomas Zilli, Nicholas Van As, Shankar Siva, Andrei Fodor et al. “Metastasis-directed Therapy in Treating Nodal Oligorecurrent Prostate Cancer: A Multi-institutional Analysis Comparing the Outcome and Toxicity of Stereotactic Body Radiotherapy and Elective Nodal Radiotherapy.” European urology (2019).
3. Mattei, Agostino, Frank G. Fuechsel, Nivedita Bhatta Dhar, Sebastian H. Warncke, George N. Thalmann, Thomas Krause, and Urs E. Studer. “The template of the primary lymphatic landing sites of the prostate should be revisited: results of a multimodality mapping study.” European urology53, no. 1 (2008): 118-125.
4. Granfors, Torvald, Hans Modig, Jan-Erik Damber, and Radisa Tomic. “Long-term followup of a randomized study of locally advanced prostate cancer treated with combined orchiectomy and external radiotherapy versus radiotherapy alone.” The Journal of urology 176, no. 2 (2006): 544-547.
5. Roach, Mack, Jennifer Moughan, Colleen AF Lawton, Adam P. Dicker, Kenneth L. Zeitzer, Elizabeth M. Gore, Young Kwok et al. “Sequence of hormonal therapy and radiotherapy field size in unfavourable, localised prostate cancer (NRG/RTOG 9413): long-term results of a randomised, phase 3 trial.” The Lancet Oncology 19, no. 11 (2018): 1504-1515.
