Barcelona, Spain (UroToday.com) In the STAMPEDE study, low metastatic burden was determined to be predictive of overall survival (OS) benefit when radiation therapy (RT) was added to standard of care (SOC) therapy in men with newly diagnosed metastatic hormone-sensitive prostate cancer (mHSPC).1 This benefit was not observed for patients with high burden metastatic disease. This analysis was performed using the CHAARTED clinical trial definition of low and high volume disease.2 In this abstract, STAMPEDE investigators sought to better understand which patients benefit from the addition of RT to SOC treatment for newly diagnosed mHSPC. Specifically, they aimed to answer the following questions: 1) Does prostate RT + SOC benefit over SOC alone in patients with only-regional lymph node (M1a) or visceral metastases (M1c)? 2) Is bone metastasis count on bone scan predictive of benefit from prostate RT + SOC over SOC alone?
Patients randomized to androgen deprivation therapy (ADT) (± docetaxel) vs RT + ADT (± docetaxel) were studied. Metastatic site, distribution, and number were evaluated based on conventional imaging and used to explore treatment effects to refine the metastatic burden definition. Results focused on the trial’s key outcome measures, OS and failure-free survival (FFS), analyzed using standard survival analysis methods. HR < 1 indicates benefit associated with RT + SOC over SOC alone.
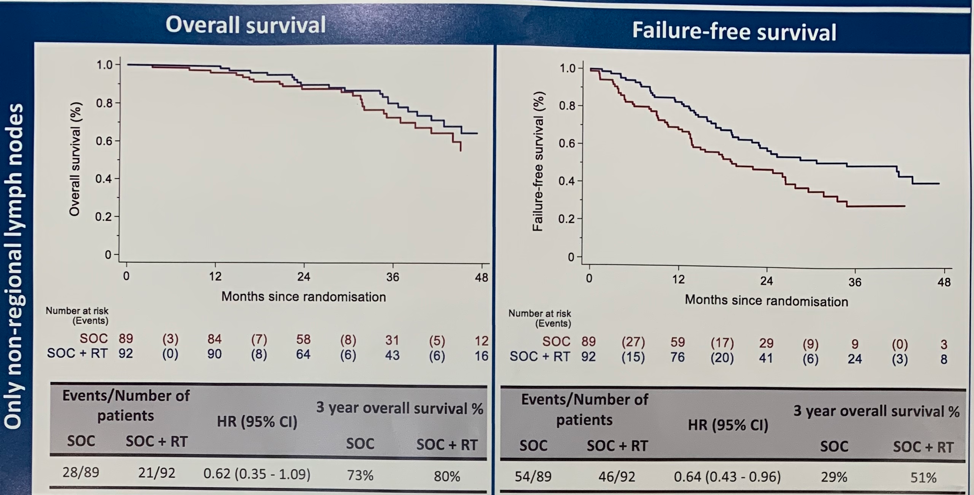
Among patients with only non-regional lymph node metastases, there was a significant improvement in FFS (HR 0.64, 0.43-0.96) and a trend towards improvement in OS (HR 0.62, 0.35-1.09) with the addition of RT to SOC therapy.
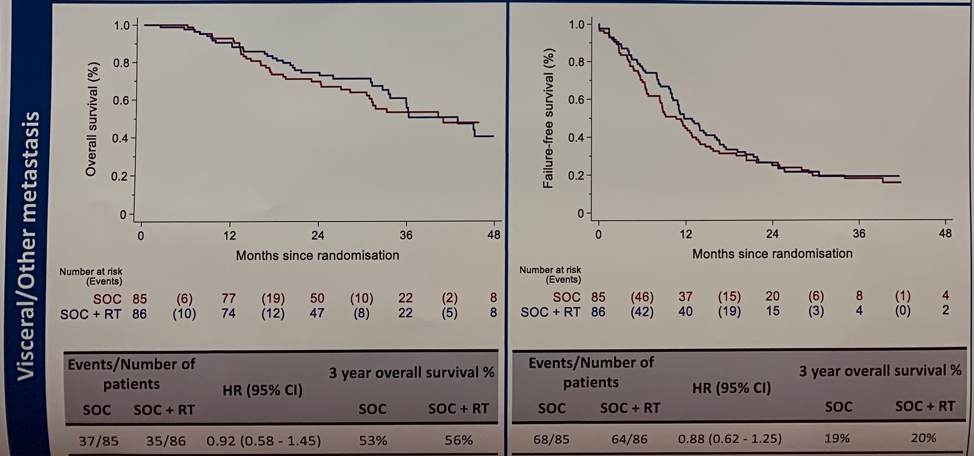
In contrast, among patients with visceral/other metastases, there was no improvement in FFS or OS for patients who received RT + SOC over SOC alone.
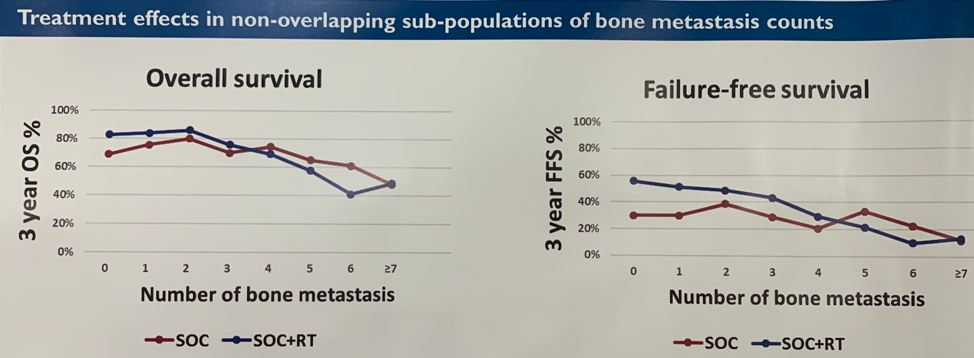
Next, the authors sought to understand whether the number of bone metastases on bone scan is predictive of benefit from prostate RT when added to SOC therapy. They found that bone metastasis count based on bone scan is predictive of OS and FFS benefit associated with RT + SOC. Improved FFS and OS was apparent in patients with < 4 bone metastases. This effect was independent of the anatomic location of bone lesions.
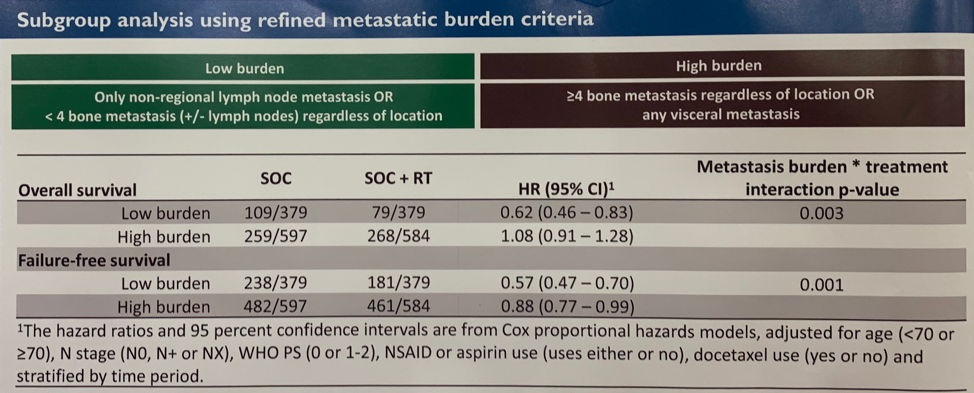
Exploratory subgroup analysis using criteria informed by this study found that prostate RT + SOC improved OS (treatment interaction p-value = 0.003) and FFS (treatment interaction p-value 0.001) in patients with only non-regional lymph nodes or < 4 bone metastases regardless of location and no visceral metastases over SOC alone.
Presented by: Syed Adnan Ali, MBBS, Clinical Research Fellow at the University of Manchester
Written by: Jacob Berchuck, MD, Medical Oncology Fellow at the Dana-Farber Cancer Institute (Twitter: @jberchuck) at the 2019 European Society for Medical Oncology annual meeting, ESMO 2019 #ESMO19, 27 Sept – 1 Oct 2019 in Barcelona, Spain
References:
1. Parker CC, James ND2, Brawley CF, et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. Lancet. 2018 Dec 1;392(10162):2353-2366.
2. Sweeney CJ, Chen YH, Carducci M, et al. Chemohormonal Therapy in Metastatic Hormone-Sensitive Prostate Cancer. N Engl J Med. 2015;373(8):737-746.
