Athens, Greece (Urotoday.com) Focal therapy can be defined as treatment of a specific focus (targeted ablation or limited defined region -quadrant-ablation or hemi-ablation).
This discussion focused on high-intensity focused ultrasound (HIFU) modality. This entails ultrasound waves delivered transrectally from a spherical transducer. The high-intensity waves converge to a focal point and cause hyperthermia and damage to the tissue. The mechanism of action consists of three effects:
- Thermal effect – focal thermal induction and rapid rise in temperature (>80 Celsius)
- Mechanical effect – generation of gas bubbles, collapse of cavities, and rupture of cell walls
- Tissue effect – coagulation necrosis which occurs immediately, an inflammatory response, which occurs after 7 days, and an induction of fibrosis, which occurs after 14 days
HIFU for the treatment of the entire gland has demonstrated adequate long-term oncologic outcomes for localized prostate cancer. The recurrence free survival at 5 years was 73% and secondary therapy free survival was 84%, 72%, and 45% for low, intermediate and high-risk disease, respectively.1 The various HIFU devices are shown in Table 1:
Table 1 – HIFU devices:
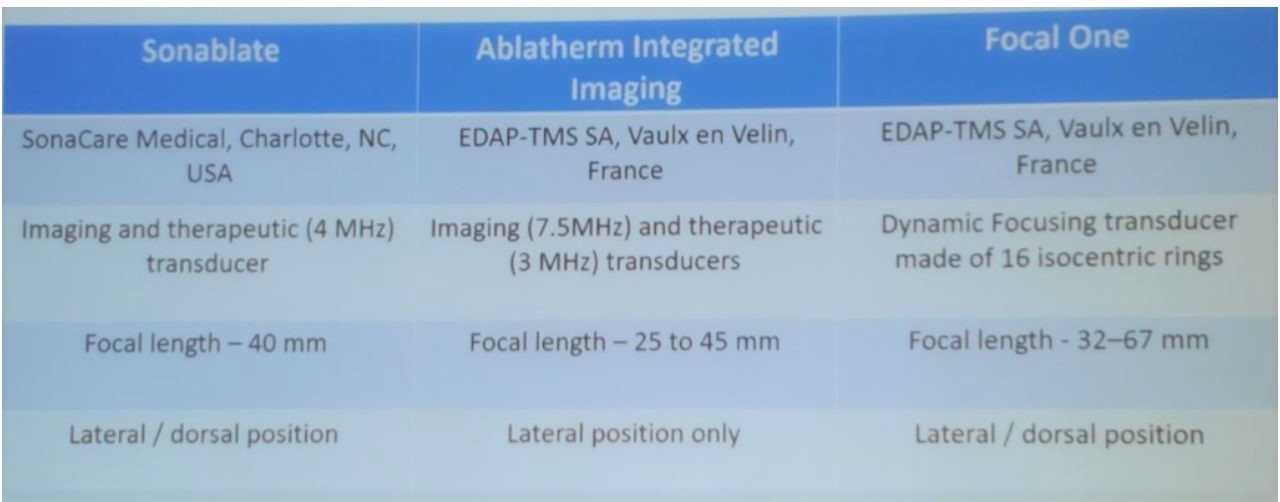
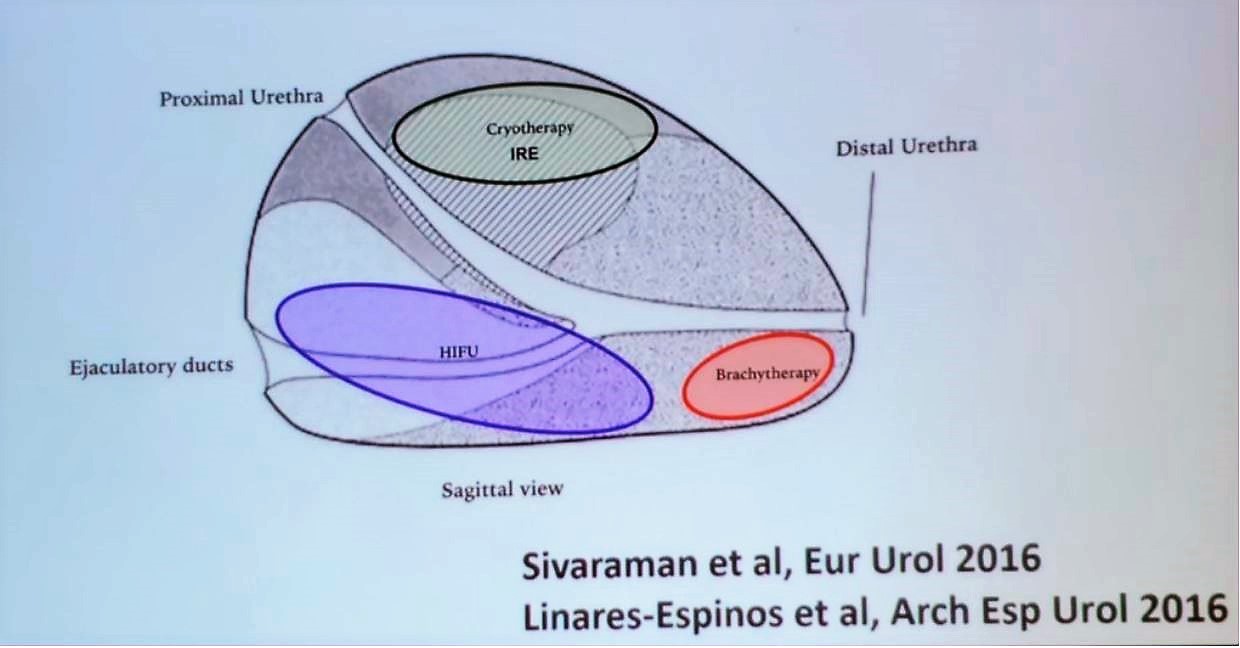
Figure 1 – Which focal therapy to use according to the prostate tumor location:
Summarizing his talk, Dr. Vallancien stated that we are still lacking long-term cancer control data with focal therapy, and the outcomes need to be improved. Focal therapy represents a promising alternative to treat intermediate-risk disease of Gleason 3+4, or low-risk tumors without an indication for active surveillance. In selected patients, hemiablation combined with mpMRI represents an accurate treatment option of the index lesion.
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New York, USA, Twitter: @GoldbergHanan at the 39th Congress of the Société Internationale d’Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:
1. Barret E, Ahallal Y, Sanchez-Salas R, et al. Morbidity of Focal Therapy in the Treatment of Localized Prostate Cancer. European Urology 2013; 63(4): 618-22.
2. El Fegoun AB, Barret E, Prapotnich D, et al. Focal therapy with high-intensity focused ultrasound for prostate cancer in the elderly. A feasibility study with 10 years follow-up. International braz j urol : official journal of the Brazilian Society of Urology 2011; 37(2): 213-9; discussion 20-2.
3. Garcia-Barreras S, Sanchez-Salas R, Sivaraman A, et al. Comparative Analysis of Partial Gland Ablation and Radical Prostatectomy to Treat Low and Intermediate Risk Prostate Cancer: Oncologic and Functional Outcomes. Journal of Urology 2018; 199(1): 140-6.
4.Ganzer R, Arthanareeswaran VKA. Which technology to select for primary focal treatment of prostate cancer?-European Section of Urotechnology (ESUT) position statement. 2018; 21(2): 175-86.
