Basel, Switzerland (UroToday.com) Dr. Declan Murphy provided a discussion on the node-positive prostate cancer session in the Advanced Prostate Cancer Consensus Conference (APCCC) in Basel, Switzerland. He began by discussing the staging of high-risk/locally advanced prostate cancer. According to the EAU guidelines, there is a strong recommendation to perform metastatic screening including at least a cross-sectional abdominopelvic imaging and a bone scan.1 The definition of pelvic clinical node-positive disease by CT criteria include:
- 8 mm short axis of a round lymph node
- 10 mm in an oval lymph node
CT scan performs very poorly for staging pelvic lymph nodes with a sensitivity of 11-13% but has a high specificity of 93-94%. The alternate option of MRI also performs poorly for staging with a sensitivity of 39-56% and a specificity of 89-94%.2
There is only limited evidence supporting the role of radical prostatectomy for clinical node-positive patients. Therefore, the EAU guidelines recommend offering radical prostatectomy to patients with high risk locally advanced prostate cancer (cT3b-T4 N0 or any T N1) only as part of multimodal therapy. An extended pelvic lymph node dissection (ePLND) should be performed in these patients according to the EAU guidelines. There are only studies supporting the role of radical prostatectomy in these specific patients.
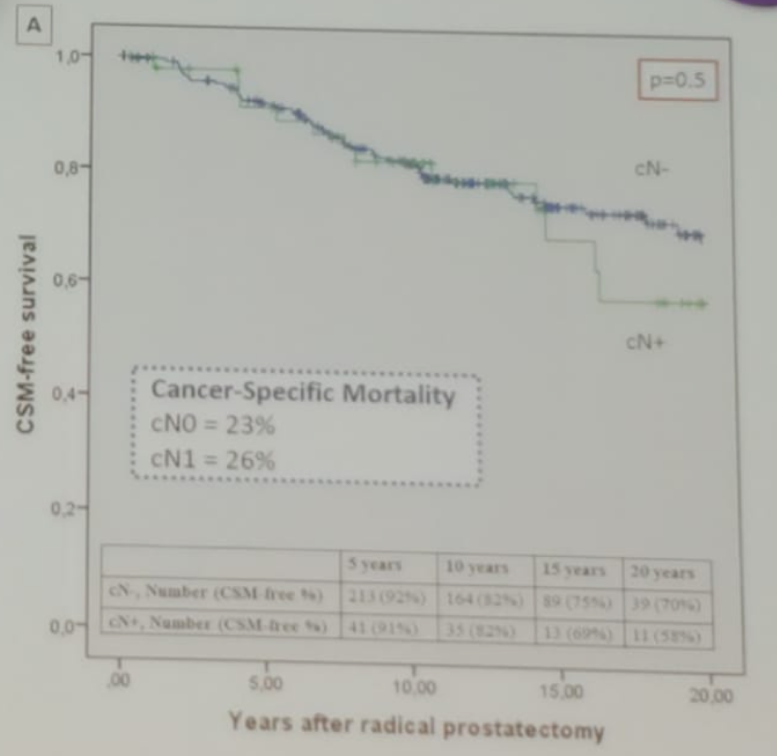
In the first study by Mochini M.,3 302 patients underwent radical prostatectomy with ePLND between 1988 and 2003. All patients were node-positive on final pathology, with only 17% being clinical node positive before surgery, and 83% were defined as a clinically node-negative disease (cN0). The median follow-up time was 17.4 years and the median number of nodes removed in surgery was 13. The results demonstrated no difference in cancer-specific mortality between cN0 and cN1 patients (figure 1). On multivariable analysis, Gleason 8 disease and the number of positive nodes removed predicted survival, but cN status did not predict survival, and so the authors concluded that cN+ status should not be a contraindication to surgery.
Figure 1 – Cancer-specific survival between patients with cN0 and cN1 undergoing radical prostatectomy:
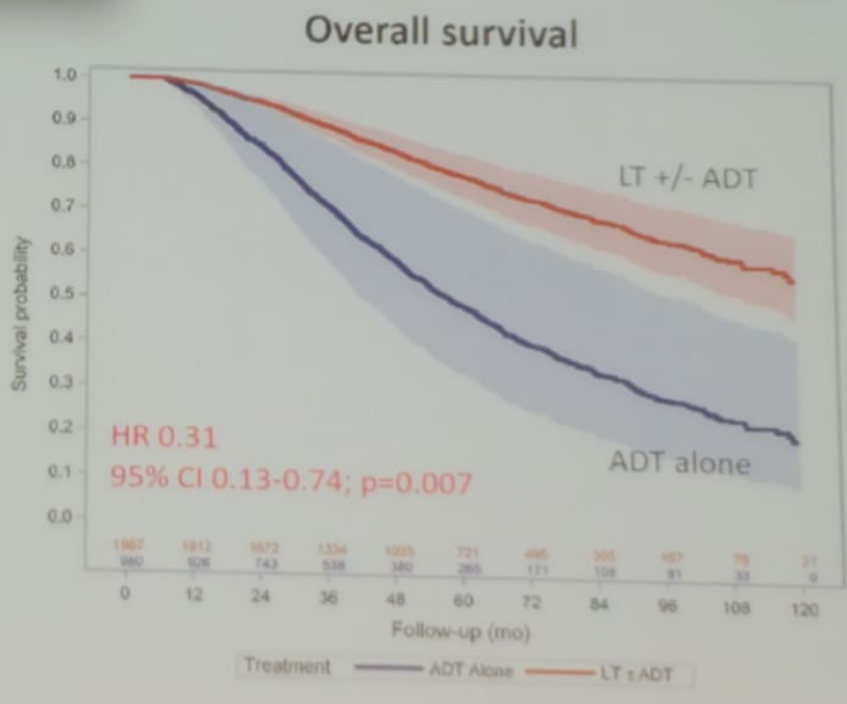
In the second study, using the national cancer database (NCDB) between 2003 and 2011, more than 2900 cN1 patients were assessed with patients receiving local therapy (radiation or surgery) +/- androgen deprivation therapy (ADT) were compared to those who received ADT alone.4 Using instrumental variable analysis, the authors demonstrated that patients treated with local therapy and ADT had significantly improved overall survival with a 71% survival benefit (HR 0.31, 95% CI 0.13-0.74, p=0.007) (Figure 2). When comparing the type of local therapy (surgery vs. radiotherapy) no significant survival benefit was noticed (HR 0.54, 95% CI 0.19-1.52, p=0.2).
Figure 2 – Overall survival compared between patients who received local therapy + ADT vs. those who received only ADT:
Next, Dr. Murphy discussed the use of PET PSMA in the diagnosis of clinical node-positive disease. Primary PET PSMA has a sensitivity of 77% and a specificity of 97% in lymph-node staging.5 According to the EAU guidelines, novel imaging is more sensitive than conventional imaging modalities, however, the benefit of detecting metastases earlier is still unclear. Once diagnosed, it is still not clear if PET-only diagnosed metastases should be treated systematically, or with aggressive local and metastases directed therapy. There is currently an ongoing randomized controlled trial evaluating the impact of these management strategies (the proPSMA trial).6 In this multicenter study 300 patients with high risk localized prostate cancer will be randomized to either conventional imaging (CT and bone scan) or to PET PSMA. The endpoint includes the accuracy of diagnosis and management impact, and this will be presented in the EAU meeting in 2020.
There are several considerations that need to be taken into account when trying to answer the discussed questions:
- If conventional imaging is negative, should we abandon the standard of care?
- Should we try harder to get tissue diagnosis?
- How should the impact of management be assessed?
- Can prospective trials embrace novel imaging?
Dr. Murphy concluded his talk with two take-home messages:
- The conventional imaging performs poorly for staging clinical node status. There is some low-quality evidence to support surgery for clinically node-positive prostate cancer, but this needs to be discussed within a multimodal framework.
- It is self-evident that PSMA PET has superior sensitivity and specificity in higher-risk prostate cancer patients. The impact of management will need to be evaluated, and this opens an option for radio-guided surgery possibilities in the near future.
Presented by: Declan G. Murphy, MB, BCH, BaO, FRACS, FRCS, Associate Professor, Urologic Oncology, Prostate Cancer, Robotic Surgery, University of Melbourne
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New-York, USA @GoldbergHanan at the 2019 Advanced Prostate Cancer Consensus Conference (APCCC) #APCCC19, Aug 29 – 31, 2019 in Basel, Switzerland
References:
- EAU prostate cancer guidelines 2019
- Briganti A. et al. Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. European Urology. 2012 Mar;61(3):480-7.
- Mochini M. et al. Natural History of Clinical Recurrence Patterns of Lymph Node-Positive Prostate Cancer After Radical Prostatectomy. European Urology 2016 Jan;69(1):135-42.
- Seisen et al. Efficacy of Local Treatment in Prostate Cancer Patients with Clinically Pelvic Lymph Node-positive Disease at Initial Diagnosis. European Urology 2018. https://doi.org/10.1016/j.eururo.2017.08.011.
- Perera et al. Gallium-68 Prostate-specific Membrane Antigen Positron Emission Tomography in Advanced Prostate Cancer—Updated Diagnostic Utility, Sensitivity, Specificity, and Distribution of Prostate-specific Membrane Antigen-avid Lesions: A Systematic Review and Meta-analysis. European Urology. 2019. https://doi.org/10.1016/j.eururo.2019.01.049.
- Hofman MS. Et al. PSMA PET/CT imaging for primary staging of intermediate and high-risk PCa. BJU International. 2019. https://doi.org/10.1111/bju.14856
