Basel, Switzerland (UroToday.com) At the Advanced Prostate Cancer Consensus Conference (APCCC) 2019 session on PSA recurrence after radical local therapy and oligometastatic prostate cancer, Dr. Christopher Evans from UC-Davis discussed the management of men with PSA recurrence or persistence after radical prostatectomy. Dr. Evans started by highlighting that the AUA definition of biochemical recurrence is remission after prostatectomy defined as nadir PSA <0.2 ng/mL. The NCCN defines biochemical recurrence as a PSA persistence/recurrence after radical prostatectomy such that the PSA fails to fall to undetectable levels (PSA persistence) or undetectable PSA after radical prostatectomy with a subsequent detectable PSA that increases on two or more determinations (PSA recurrence).
Between 5-20% of men continue to have persistent PSA after radical prostatectomy, defined in most studies as detectable post-radical prostatectomy PSA of >0.1 ng/mL within 4-8 weeks after surgery. This may result from persistent local disease, pre-existing metastases or residual benign prostate tissue, most commonly at the bladder neck. Dr. Evans notes that in his experience a PSA > 0.1 ng/mL is not a residual benign disease. The first steps in the setting of PSA persistence are to repeat a PSA for validation and follow at 2-3 month intervals to an initial read on the etiology for persistence. A PSA persistence has important implications on long-term outcomes: at 15-years after radical prostatectomy, MFS and CSS is 53.0% vs 93.2% and 75.5% vs 96.2%, for persistent vs undetectable PSA, respectively.1 On multivariable analysis, higher preoperative PSA, more advanced pathologic tumor stage, pathologic Gleason Group 3-5, positive surgical margins, and pN1 was associated with an increased risk of persistent PSA. Furthermore, after propensity score matching between patients with salvage radiation therapy vs patients with no salvage radiation therapy, the CSS at 10 years after radical prostatectomy was 93.7% vs 81.6% in the entire cohort (p < 0.01).
With regards to biochemical recurrence, Dr. Evans highlighted the classic JAMA paper by Dr. Pound while he was at Johns Hopkins Hospital.2 This study was a retrospective review of 1997 men who underwent radical prostatectomy between 1982 and 1997; of these men, 315 (15%) developed biochemical PSA level elevation and 11 underwent early hormone therapy after the recurrence and were not included in the study. The 5-year metastatic progression-free survival rate was 64% among 304 BCR patients who were observed until metastatic progression. In a recent systematic review assessing the prognostic value of biochemical recurrence following treatment with curative intent, only approximately 30% of patients with BCR after primary surgery develop clinical recurrence, with only 16.4% dying from their disease.3 Based on this review, there was a proposal to stratify patients into (i) EAU low-risk BCR: PSA doubling time >1 year and pGS <8 for radical prostatectomy, and (ii) EAU high-risk BCR: PSA doubling time <=1 year or pGS 8-10 for radical prostatectomy.
As has also presented at this conference, there has been many advances in the imaging-space for patients with biochemical recurrence. A recent updated systematic review of PSMA PET-CT scan this year assessed 37 articles (n = 4790 patients) and found that for patients with biochemical recurrence, positive 68Ga-PSMA PET scans increased with higher pre-PET PSA levels:4
- PSA 0-0.19 ng/mL: 33%
- PSA 0.2-0.49 ng/mL: 45%
- PSA 0.5-0.99 ng/mL: 59%
- PSA 1-1.99 ng/mL: 75%
- PSA ≥2ng/ml: 95%
Importantly, there were no significant differences in positivity noted between Gleason sums ≤7 and ≥8 diseases. On per-node analysis, there was high sensitivity (75%) and specificity (99%) observed.
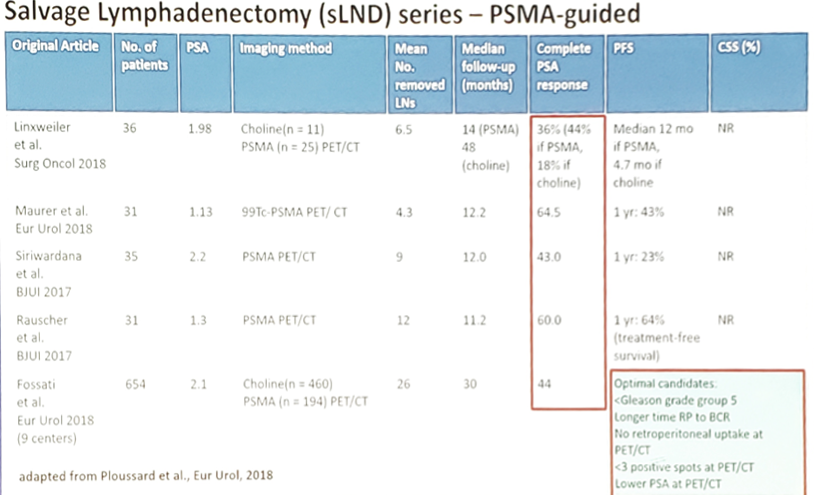
In addition to salvage radiotherapy for biochemical recurrence/persistent PSA, there has been anecdotal evidence for salvage lymph node dissection. A systematic review from 2018 demonstrated that among 27 studies,5 salvage lymph node dissection was performed by open or laparoscopic approach with <10% of grade 3 or more complication rate. Over a mean follow-up of 29.4 month, complete biochemical response after salvage lymph node dissection was achieved in 13-79.5%of cases, and the 2- and 5-year biochemical progression-free survival rates ranged from 23% to 64% and from 6% to 31%, respectively.
The following table highlights the salvage lymphadenectomy series with PSMA guidance:
Dr. Evans concluded this talk with several summary points:
- PSA persistence >0.1 ng/mL has a poor prognosis but salvage radiation therapy is beneficial
- PSA recurrence has several definitions – the new EAU guidelines move from absolute value to risk groups
- New imaging has a relevant and evolving role
- EAU low risk is at a small risk of metastatic progression or cancer-specific mortality
- Salvage radiation therapy with ADT should be given in EAU high-risk patients
- Salvage surgical approaches are immature and should be considered cautiously
References:
- Preisser F, Chun FKH, Pompe RS, et al. Persistent Prostate-Specific Antigen After Radical Prostatectomy and Its Impact on Oncologic Outcomes. Eur Urol 2019 Jul;76(1):106-114.
- Pound CR, Partin AW, Eisenberger MA, Chan DW, Pearson JD, Walsh PC. Natural history of progression after PSA elevation following radical prostatectomy. JAMA 1999 May 5;281(17):1591-1597.
- Van Den Broeck T, van den Bergh RCN, Arfi N, et al. Prognostic Value of Biochemical Recurrence Following Treatment with Curative Intent for Prostate Cancer: A Systematic Review. Eur Urol 2019 Jun;75(6):967-987.
- Perera M, Papa N, Roberts M, et al. Gallium-68 Prostate-specific Membrane Antigen Positron Emission Tomography in Advanced Prostate Cancer-Updated Diagnostic Utility, Sensitivity, Specificity, and Distribution of Prostate-specific Membrane Antigen-avid Lesions: A Systematic Review and Meta-analysis. Eur Urol 2019 Feb 14 [Epub ahead of print].
- Ploussard G, Gandaglia G, Borgmann H, et al. Salvage Lymph Node Dissection for Nodal Recurrent Prostate Cancer: A Systematic Review. Eur Urol 2018 Oct 31 [Epub ahead of print].
Presented by: Christopher P. Evans, MD, FACS, Chair, Department of Urologic Surgery, University California, Davis, Sacramento, California
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_md at the 2019 Advanced Prostate Cancer Consensus Conference (APCCC) #APCCC19, Aug 29 – 31, 2019 in Basel, Switzerland
