On behalf of the Young Academic Urologists (YAU) Kidney Cancer working group of the European Urological Association (EAU), a systematic review and quantitative synthesis of the impact of suture techniques during laparoscopic and robot-assisted partial nephrectomy was recently published in the British Journal of Urology International.1 Interesting findings of the study included that running suture, particularly using barbed wires, has shortened the operating and ischemia times. A further advantage could derive from avoiding a double-layer suture. It is known that the goal of partial nephrectomy is the complete tumor excision with negative margins, maximal functional preservation, and avoidance of complications. Resection and renorrhaphy techniques actually affect the amount of vascularized parenchyma preserved, which represents a major determinant of ultimate renal function.
Renorrhaphy techniques during minimally-invasive partial nephrectomy have evolved due to several reasons. During the earlier laparoscopic series, renorrhaphy was focused on minimizing complications by accurate hemostasis and closure of the collecting system. Nowadays, the concept of “nephron-sparing renorrhaphy” aims to maximize the vascularized parenchymal volume and thus the ultimate renal function. Despite the important relationship between the suture technique and the functional outcomes of partial nephrectomy, the urological guidelines do not provide any recommendations about the optimal renorrhaphy technique, since evidence on the preferred technique remains inconclusive.
On behalf of the YAU Kidney Cancer working group again we published on European Urology Oncology the first systematic assessment on the impact of suture technique on renal function during partial nephrectomy. With the report, we sought to pool the available literature data on the impact of suture techniques on renal function after minimally invasive partial nephrectomy.
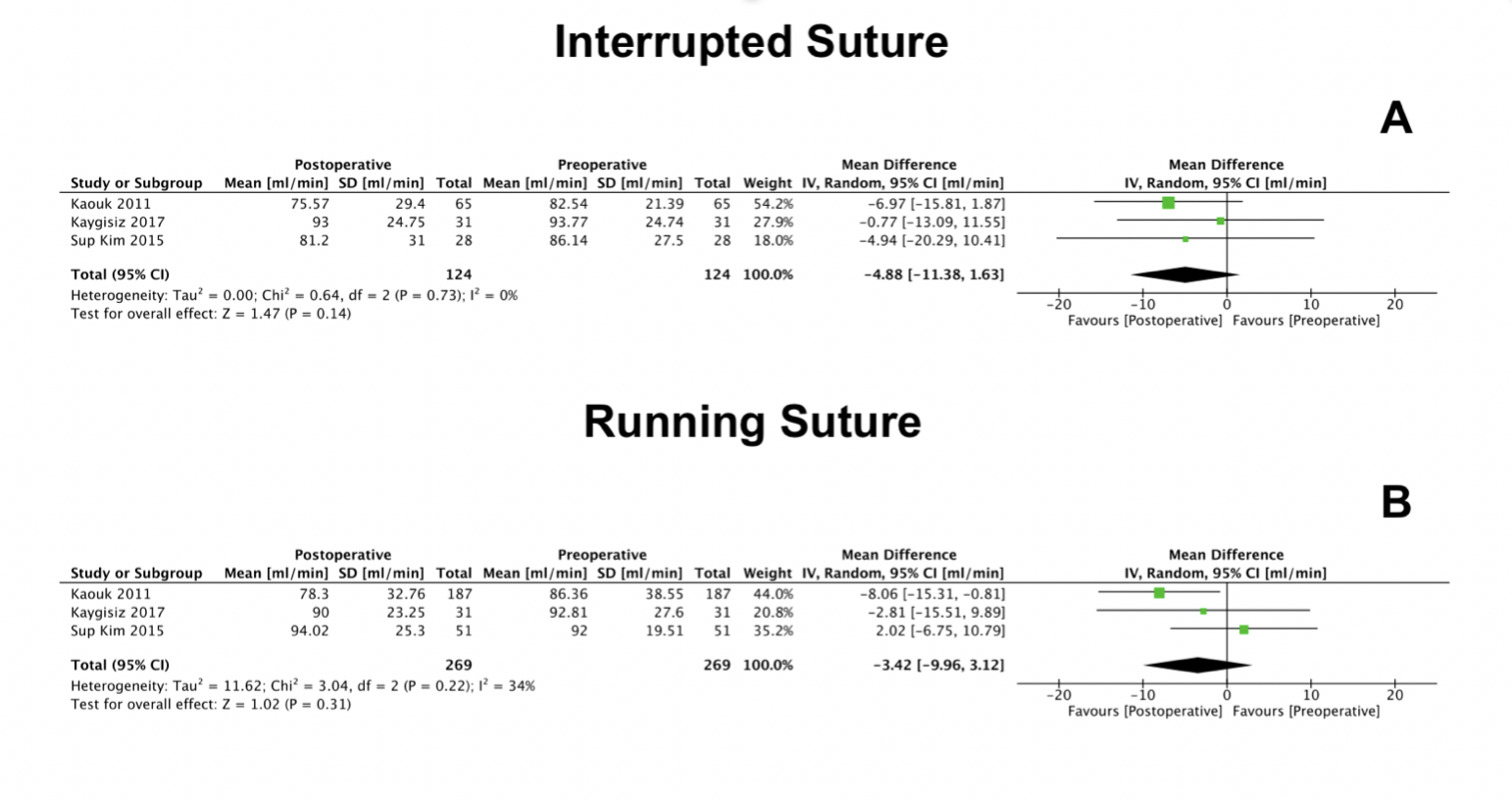
In our previous publication on perioperative outcomes of surgery, interrupted renorrhaphy technique resulted in higher operative time, ischemia time, and complications relative to the running suture technique. In the present report, we were able to perform a quantitative synthesis of three studies comparing interrupted versus running suture, which included data on estimated glomerular filtration rate (eGFR) for a total of 124 versus 269 patients. Postoperative eGFR was assessed between the date of discharge and 1 month postoperatively. No significant differences were found between pre- and postoperative eGFR in both patients who received an interrupted suture (Figure 1A) or those who received a running suture (Figure 1B). A similar renal functional outcome was observed despite longer ischemia times for interrupted suture, confirming the current literature showing a low impact on renal function of longer ischemia intervals. On the contrary, we believe that running sutures possibly tend to incorporate a larger amount of healthy parenchyma, thus smoothing the differences in renal function; however, further studies are needed to confirm this statement.
Single-layer techniques have reported allowing for better perioperative outcomes and a non-significantly higher rate of postoperative complications when compared to standard double-layer techniques. In the quantitative analysis comparing single- versus double-layer renorrhaphy including pre- and postoperative GFR data (321 vs 199 patients), we found a benefit in functional outcomes in favor of the single-layer technique (Figures 1C and 1D). Among the three studies included in the quantitative synthesis, the one performed by Bahler et al. was particularly underlined, which investigated the feasibility of omitting the cortical renorrhaphy during robotic partial nephrectomy. Without differences in the postoperative complications, Bahler and colleagues reported a significantly lower percentage of volume loss of the operated kidney (assessed by software-based volumetric assessment on computed tomography scans) when omitting one renorrhaphy layer. This finding was postulated to be secondary to the hypoperfusion of the parenchyma that occurs during cortical renorrhaphy. According to the available evidence as well as expert opinions, the cortical rather than the medullary layer could be omitted during single-layer renorrhaphy. On the contrary, the use of a single-layer technique has remained questionable and with limited diffusion as it prevents re-approximation of the renal cortical rims. The choice often depends on the tumor growth pattern. Moreover, the volume of perilesional healthy parenchyma excised will have an impact on the renorrhaphy.
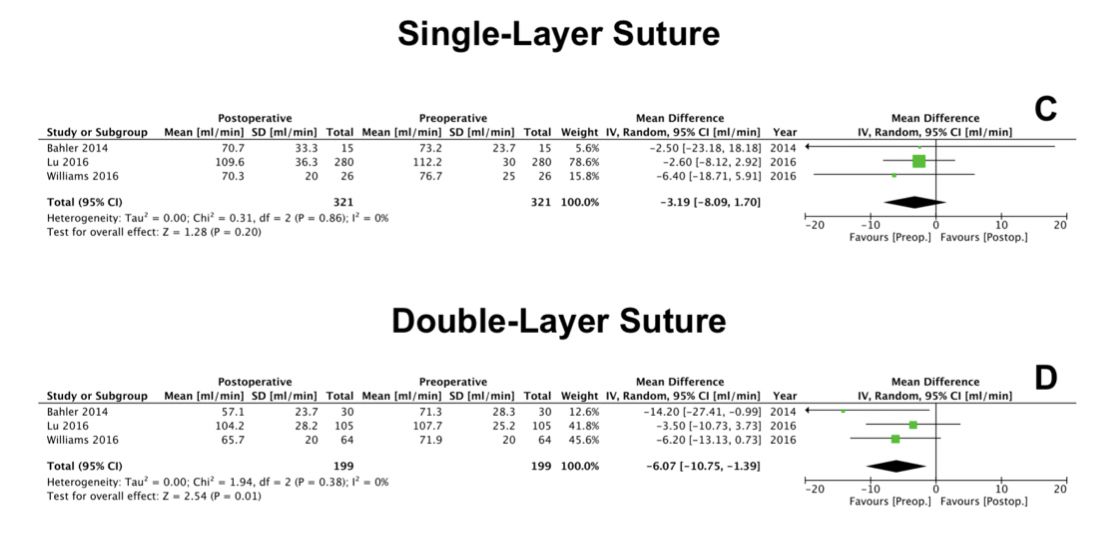 In our recent publication commented herein, it was acknowledged that only a limited number of studies was considered. Moreover, we did not account for tumor complexity. Furthermore, the available literature allowed for early postoperative functional data assessment only. It is known that functional recovery occurs at longer follow-up, and the clinical relevance of the benefit reported favoring single-layer suture technique remains questionable. These limitations compromised the quality of the evidence. Notwithstanding these limitations, our study represents the first pooled analysis of the literature able to reference the impact of renorrhaphy on renal function following partial nephrectomy. The analysis suggests that “less is more” for renorrhaphy, that is, single-layer renorrhaphy techniques may lead to better postoperative renal function. Future efforts are warranted for improving the literature evidence.
In our recent publication commented herein, it was acknowledged that only a limited number of studies was considered. Moreover, we did not account for tumor complexity. Furthermore, the available literature allowed for early postoperative functional data assessment only. It is known that functional recovery occurs at longer follow-up, and the clinical relevance of the benefit reported favoring single-layer suture technique remains questionable. These limitations compromised the quality of the evidence. Notwithstanding these limitations, our study represents the first pooled analysis of the literature able to reference the impact of renorrhaphy on renal function following partial nephrectomy. The analysis suggests that “less is more” for renorrhaphy, that is, single-layer renorrhaphy techniques may lead to better postoperative renal function. Future efforts are warranted for improving the literature evidence.
Written by: Riccardo Bertolo, MD – Young Academic Urologist, Renal Cancer Working Group – San Carlo di Nancy Hospital, Rome, Italy
