Barcelona, Spain (UroToday.com) Platinum-based chemotherapy remains the standard of care for patients with locally advanced or metastatic urothelial carcinoma. Despite the use of first-line PD-1/PD-1L inhibitors, 71–76% of patients who are cisplatin-ineligible do not respond to treatment. Enfortumab vedotin is an antibody-drug conjugate targeting Nectin-4, which is highly expressed in metastatic urothelial carcinoma. Enfortumab vedotin monotherapy data are encouraging, initially presented at ASCO 2019, demonstrating a 44% response rate (12% complete response). Perhaps combination therapy may provide additional benefit – the working hypothesis is that combination enfortumab vedotin plus pembrolizumab is feasible, safe, and may lead to improved responses compared to historical controls in the first-line cisplatin-ineligible setting. At the 2019 European Society for Medical Oncology annual meeting (ESMO) proffered paper session, Dr. Hoimes and colleagues presented initial data on a cohort of cisplatin-ineligible patients receiving first line enfortumab vedotin + pembrolizumab.
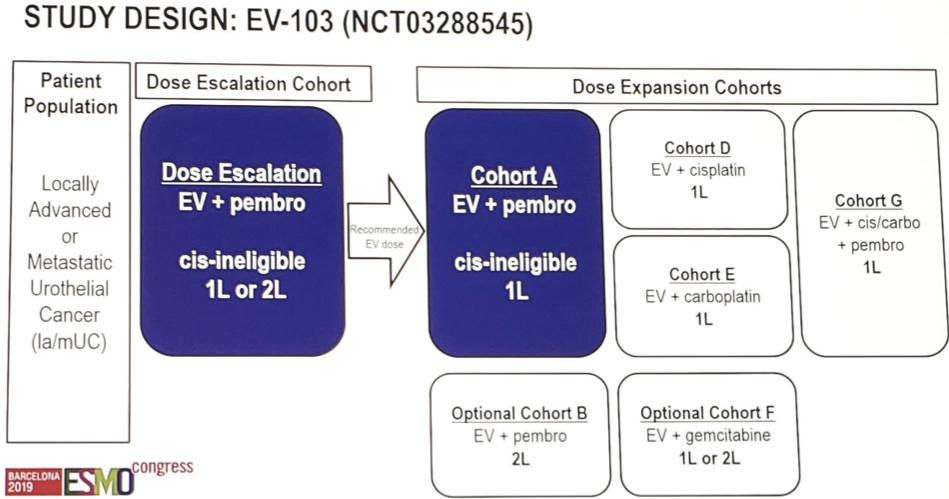
EV-103 was a phase 1b study evaluating the safety and activity of enfortumab vedotin + pembrolizumab. In the dose-escalation cohort, first-line or second-line patients received 1.0 or 1.25 mg/kg enfortumab vedotin + 200 mg pembrolizumab. Cohort A patients received the recommended dose of 1.25 mg/kg enfortumab vedotin + pembrolizumab as first-line therapy. In each 21-day cycle, enfortumab vedotin was administered on Days 1 and 8 and pembrolizumab on Day 1. The primary endpoint was safety and tolerability. The key secondary objectives were recommended enfortumab vedotin dose, antitumor activity, durable complete response, durable objective response, PFS, and overall survival (OS).
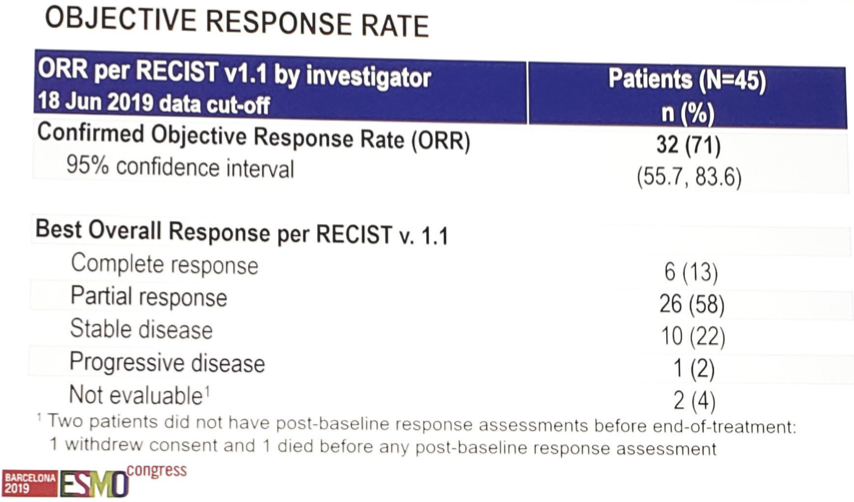
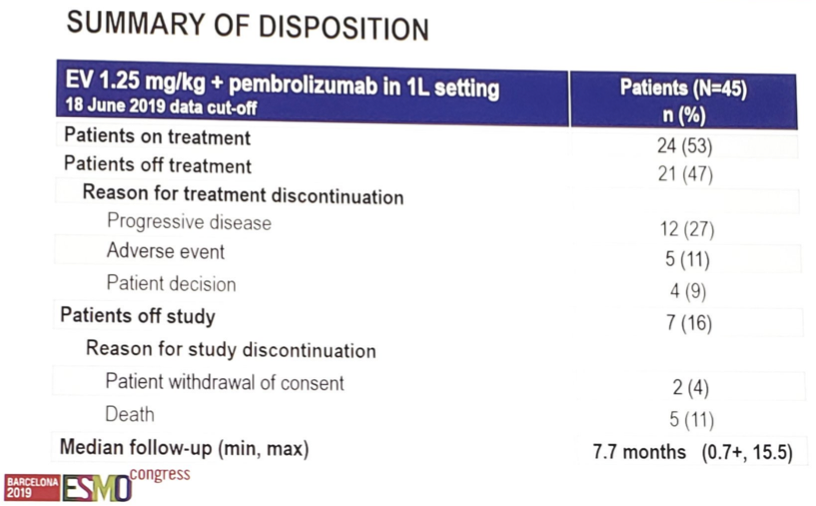
As of June 18, 2019, 45 locally advanced or metastatic urothelial carcinoma patients have been treated with enfortumab vedotin (1.25 mg/kg) + pembrolizumab in the first-line setting and completed at least 2 post-baseline scans or discontinued treatment. The median age was 69 years [range 51–90], 33% had liver metastasis, and 13% were ECOG 2. Preliminary confirmed objective response rate (ORR) per RECIST 1.1 was 71% by investigators, including a 13% complete response rate, and the durable complete response rate was 90%.
Over a median follow-up of 7.7 months (range 0.7 to 15.5), 53% of patients remained on treatment.
The most common treatment-emergent adverse events were fatigue (49%, 9% ≥Grade 3), decreased appetite (33%, 0% ≥Grade 3), alopecia (47%), and diarrhea (40%, 4% ≥Grade 3). Among adverse events of clinical interest, rash of any type occurred in 27% of patients (7% ≥Grade 3), and peripheral neuropathy of any type in 47% (4% ≥Grade 3). Overall, 4 patients (9%) discontinued treatment with enfortumab vedotin + pembrolizumab due to adverse events.
Dr. Hoimes concluded his presentation of EV-103 with the following statements:
- In first-line cisplatin-ineligible patients with locally advanced or metastatic urothelial carcinoma, enfortumab vedotin + pembrolizumab demonstrated encouraging efficacy with a tolerable and manageable safety profile
- Further evaluation of this combination is warranted
- Enfortumab vedotin + pembrolizumab has the potential to become a platinum-free option for cisplatin-ineligible patients with locally advanced or metastatic urothelial carcinoma in the first-line setting
Clinical trial identification
Presented by: Christopher J. Hoimes, DO, Assistant Professor, Department of Medicine Division of Hematology and Oncology, School of Medicine Member, GU Malignancies Program, Case Comprehensive Cancer Center, Case Western Reserve University/University Hospitals, Cleveland, Ohio
Co-Authors: J. Rosenberg 2, S. Srinivas 3, D. Petrylak 4, M. Milowsky 5, J. Merchan 6, M. Bilen 7, S. Gupta 8, A.-S. Carret 9, N. Yuan 9, A. Melhem-Bertrandt 10, T. Flaig 11
2. Memorial Sloan Kettering Cancer Center, New York, US
3. Stanford University, Palo Alto, US
4. Yale Cancer Center, New Haven, US
5. University of North Carolina at Chapel Hill, Chapel Hill, US
6. University of Miami, Miami, US
7. Emory University Winship Cancer Institute, Atlanta, US
8.University of Minnesotta, Minneapolis, US
9. Seattle Genetics, Bothell, US
10. Astellas Pharma USA, Northbrook, US
11. University of Colorado Cancer Center
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Twitter: @zklaassen_md at the 2019 European Society for Medical Oncology annual meeting, ESMO 2019 #ESMO19, 27 Sept – 1 Oct 2019 in Barcelona, Spain
