Barcelona, Spain (UroToday.com) In this special symposium, Dr. Siefker-Radke discussed the current status and future directions of combination chemo-immunotherapy in advanced urothelial carcinoma. While the full results of IMvigor130 were unavailable at the time of this presentation, Dr. Siefker-Radke focused on the clinical and biologic rationale for combination approaches.
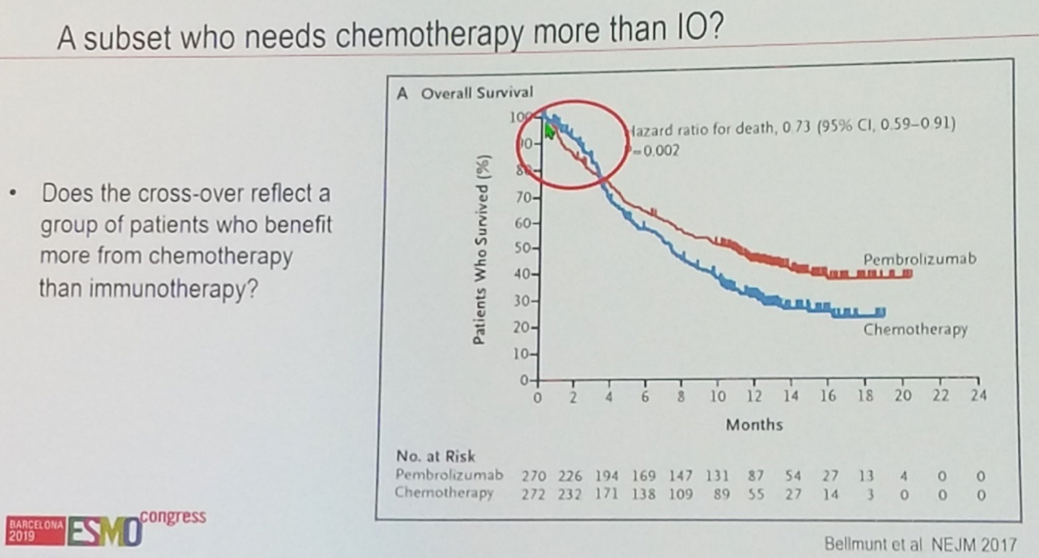
Given the unmet clinical need for certain patients who do not derive benefit from immunotherapy, it would make sense to consider chemotherapy for this group. In particular, patients with liver metastases had a lower response rate to checkpoint blockade both in IMvigor210 cohort 2 with atezolizumab and in Keynote-052 with pembrolizumab; perhaps these patients or patients with high disease burden may represent the cohort that derives early benefit from chemotherapy instead of immunotherapy as illustrated in the Kaplan-Meier plot from Keynote-052.
Furthermore, chemotherapy may augment antigen presentation. In a cohort of muscle-invasive bladder cancer patients, it was found that high frequency of CD19+ antigen presenting cells within the tumor was associated both with greater benefit from adjuvant platinum-based chemotherapy and with improved overall survival.1
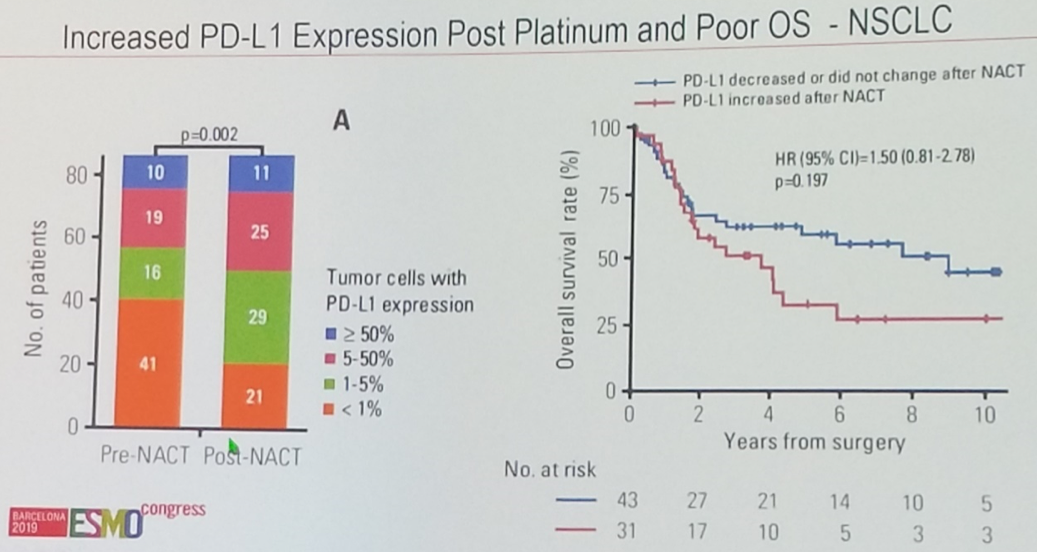
In addition, there are data to suggest that PD-L1 upregulation may be a mechanism of resistance to chemotherapy. In locally advanced non-small cell lung cancer, it was shown that PD-L1 expression increases under the selective pressure of neoadjuvant chemotherapy, and that tumors which upregulated PD-L1 in this fashion were associated with a shorter overall survival. Extrapolating to urothelial cancer, it could be hypothesized that by concomitantly blocking the PD-1/PD-L1 axis along with cytotoxic chemotherapy, this resistance could be averted.
However, there is also a rationale to avoid combining cytotoxic chemotherapy with immunotherapy given commonly-associated neutropenia and – especially in the case of gemcitabine – lymphopenia. In addition, there are data to suggest that cisplatin may actually impair dendritic cell maturation and antigen presentation.2
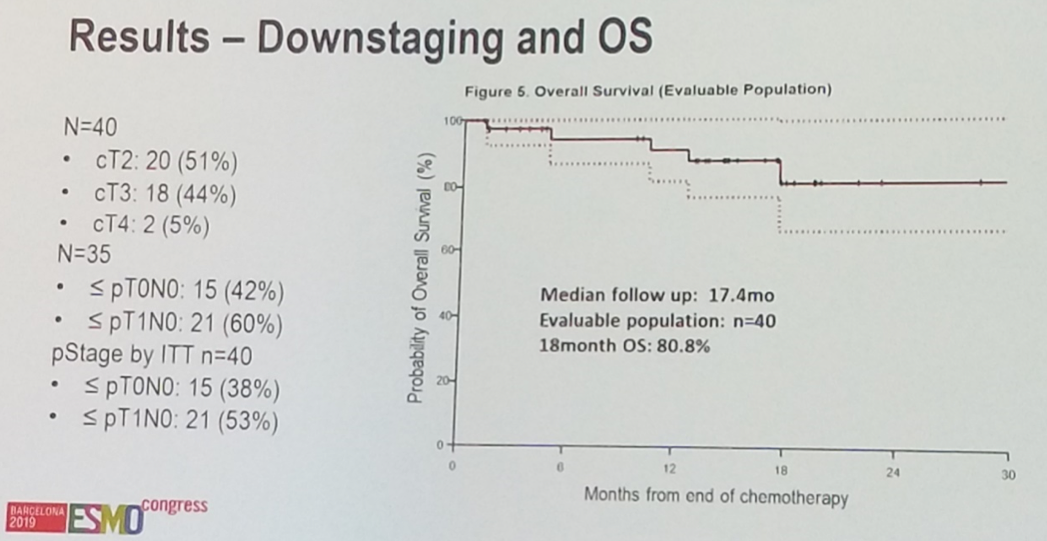
Additional studies examining the efficacy neoadjuvant chemoimmunotherapy are underway. A phase Ib/II study of gemcitabine and cisplatin with the PD-1 antibody pembrolizumab has demonstrated encouraging activity in muscle invasive bladder cancer. A total of 38% of patients achieved a pathologic complete response, and an additional 15% were down-staged to non-muscle invasive disease. Investigators found an 18-month overall survival of 80.8%, though these data are not yet mature.
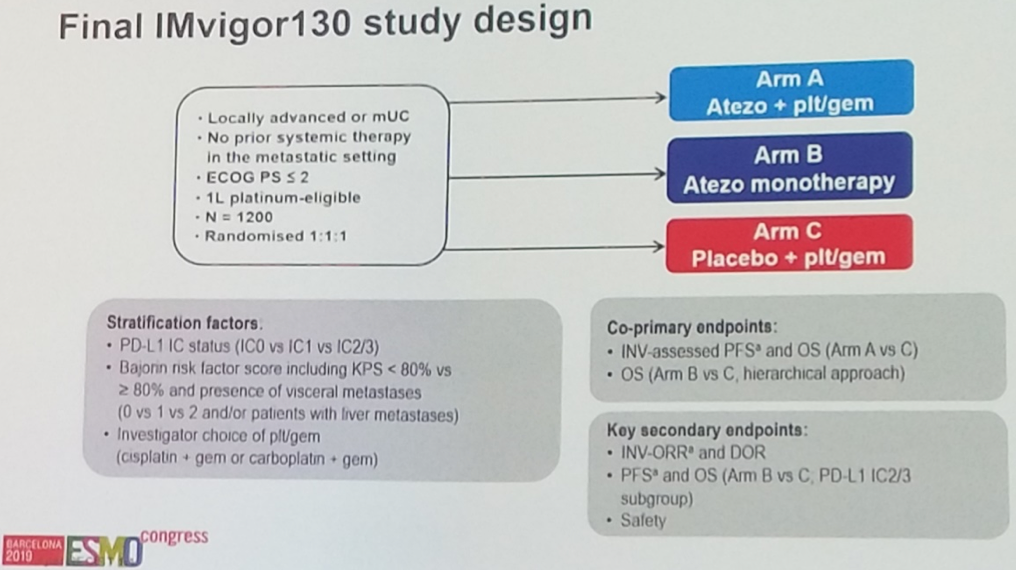
IMvigor130 was a randomized phase III trial of platinum-based chemotherapy with or without the PD-L1 antibody atezolizumab versus atezolizumab monotherapy. The study met its primary endpoint of improved progression-free survival with combination platinum-based chemotherapy and atezolizumab, though data were not yet available at the time of this presentation.
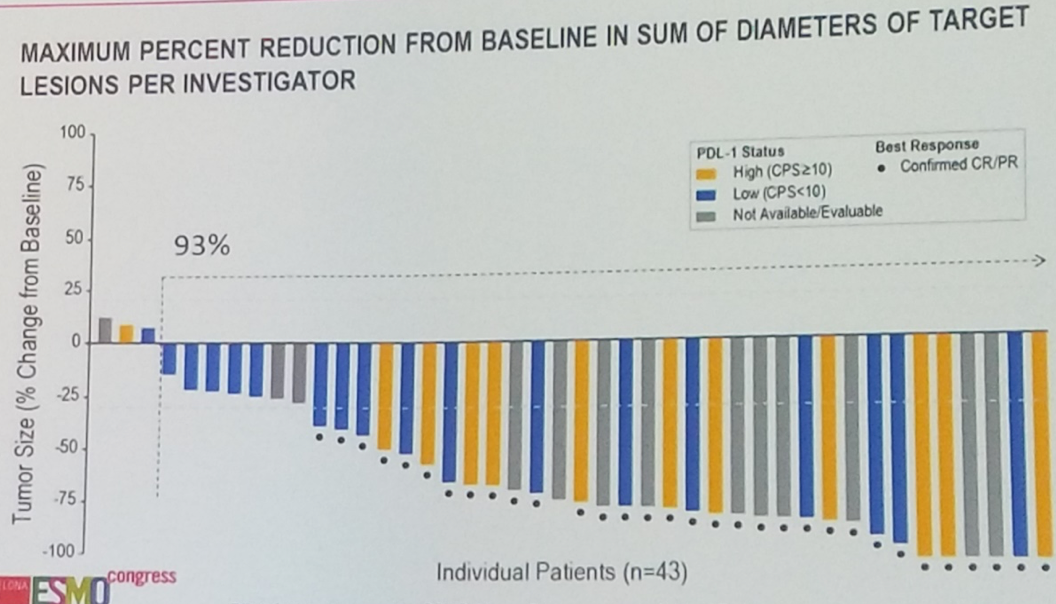
In addition to traditional cytotoxic chemotherapy, the combination of checkpoint blockade and the antibody drug conjugate enfortumab veotin generated a very impressive 71% objective response rate in the first-line metastatic setting among cisplatin-ineligible patients. Future work will examine how best to incorporate enfortumab vedotin into the treatment paradigm of metastatic urothelial cancer.
In summary, given the reported improvement in progression free survival with combination atezolizumab plus platinum-based chemotherapy, chemo-immunotherapy will likely become standard of care in the first-line setting in metastatic urothelial cancer. Future work will more closely examine the sequencing and combination of various different cytotoxic agents to maximize immunogenic cell death.
Presented by: Arlene Siefker-Radtke, MD, The University of Texas MD Anderson Cancer Center, Houston, US
References:
- Jiang Q, Fu Q, Chang Y, Liu Z, Zhang J, Xu L, Zhu Y, Wang Y, Zhang W, Xu J. CD19+ tumor-infiltrating B-cells prime CD4+ T-cell immunity and predict platinum-based chemotherapy efficacy in muscle-invasive bladder cancer. Cancer Immunology, Immunotherapy. 2019 Jan 25;68(1):45-56.
- Kim WS, Kim H, Kwon KW, Im SH, Lee BR, Ha SJ, Shin SJ. Cisplatin induces tolerogenic dendritic cells in response to TLR agonists via the abundant production of IL-10, thereby promoting Th2-and Tr1-biased T-cell immunity. Oncotarget. 2016 Jun 7;7(23):33765.
Written by: Michael Lattanzi, MD, Medical Oncology Fellow, Memorial Sloan Kettering Cancer Center, Twitter: @MikeLattanzi at the 2019 European Society for Medical Oncology annual meeting, ESMO 2019 #ESMO19, 27 Sept – 1 Oct 2019 in Barcelona, Spain
