Athens, Greece (UroToday.com) Dr. Axel Heidenreich gave a presentation on the role of salvage lymph node dissection after radical prostatectomy, in the PSMA era. It is important to remember that the oncological benefit of salvage pelvic lymph node dissection following radical prostatectomy, in the setting of oligometastatic prostate cancer is still experimental, and it should not be standardized until we have level one evidence proving its benefit.
The oligometastatic disease was initially introduced by Hallman and Weichselbaum in 1995. They defined the oligometastatic state as an intermediate state of tumor spread with limited metastatic capacity. In this unique disease state there is low volume locoregional disease spread which has a better prognosis than systemic spread. Due to these attributes, metastasis directed therapy may be effective.
The goals of salvage lymphadenectomy include:
- Improvement of cancer-specific survival
- Improvement of symptom-free-survival
- Delay initiation of systemic therapy
- Reduce treatment-associated morbidity
The prerequisites for a successful local treatment include accurate imaging which will detect early metastases, complete eradication of all oligometastatic sites, and have acceptable toxicity.
If deciding to perform salvage lymph node dissection, an extended ipsilateral template should always be done, to make sure no disease is left unremoved. In a study assessing the outcomes of performing a salvage lymph node dissection, the biochemical-free -survival after three years was 24.6% and the androgen deprivation therapy (ADT) free survival rate after three years was 43.5%.1 However, if the postoperative PSA following the initial radical prostatectomy was less than 0.2 ng/ml than the biochemical free survival free rate at three years will increase to 69%; and if it was higher than 0.2 ng/ml, it will go down to 7%.1
The technical feasibility of the procedure, whether done robotically or in standard open procedure does not always mean that it is oncologically justified. There are also complications in these procedures which should be accounted for. These include lymphorrhea, wound dehiscence, deep vein thrombosis, ileus, lymphocele requiring drainage, and hydronephrosis.2 Importantly, if there are more than two positive nodes on PET, there are data showing that salvage surgery has no benefit.3 There is actually a risk calculator that has been developed to calculate the risk of clinical recurrence within a year following the salvage procedure4 (Table 1).
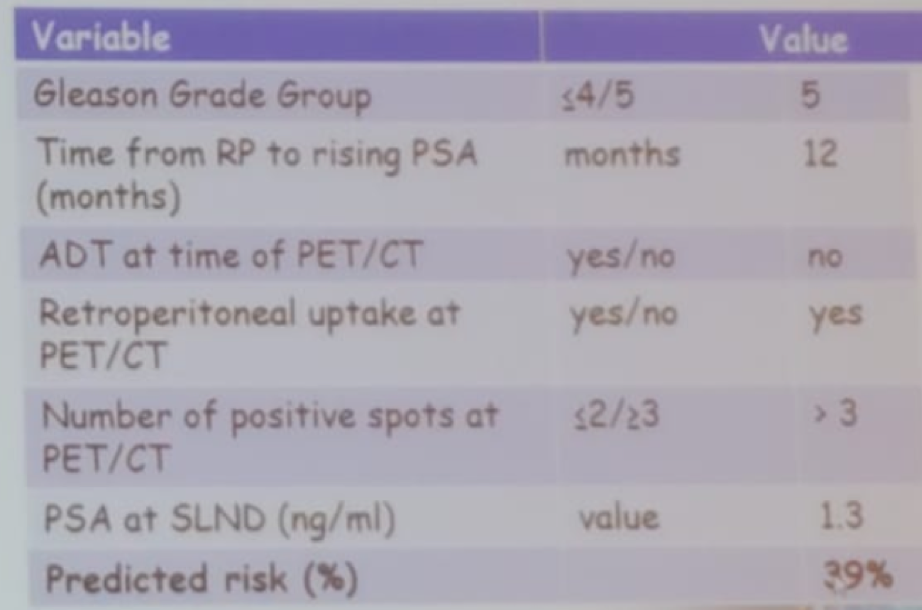
Table 1 – Risk calculator to determine the risk of recurrence within one year from salvage procedure:
Concluding his talk, Dr. Heidenreich reiterated the fact that metastasis directed therapy is still experimental and should not be regarded as standard treatment. According to the data we have today, this procedure is not justified in the following cases:
- >2 visible spots on PSMA PET/CT
- If retroperitoneal positive nodes exist
- Gleason group 5 is present
- Pathological N1 is present at the time of initial radical prostatectomy
When contemplating whether this procedure can be performed, it is recommended to use the above-mentioned risk calculator and discuss the potential outcomes with the patient.
Presented by: Axel Heidenreich, MD, Professor of Urology, Chairman, Director of the Department of Urology, Uro-Oncology, Robot-Assisted, and Specialized Urologic Surgery at the University Hospital in Cologne, Germany
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New-York, USA @GoldbergHanan at the 39th Congress of the Société Internationale d’Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:
- Porres D, Pfister D, Thissen A, et al. The role of salvage extended lymph node dissection in patients with rising PSA and PET/CT scan detected nodal recurrence of prostate cancer. Prostate cancer and prostatic diseases 2017; 20(1): 85-92.
- Ost P, Bossi A, Decaestecker K, et al. Metastasis-directed therapy of regional and distant recurrences after curative treatment of prostate cancer: a systematic review of the literature. Eur Urol 2015; 67(5): 852-63.
- Abreu A, Fay C, Park D, et al. Robotic salvage retroperitoneal and pelvic lymph node dissection for ‘node-only’ recurrent prostate cancer: technique and initial series. BJU international 2017; 120(3): 401-8.
- Fossati N, Suardi N, Gandaglia G, et al. Identifying the Optimal Candidate for Salvage Lymph Node Dissection for Nodal Recurrence of Prostate Cancer: Results from a Large, Multi-institutional Analysis. Eur Urol 2019; 75(1): 176-83.
