Athens, Greece (UroToday.com) Dr. James Eastham ended the Master class session giving a talk on the oncologic outcome and patterns of recurrence after salvage radical prostatectomy.
Biochemical failure after radiotherapy is most commonly defined using the ASTRO Phoenix definition of PSA nadir + 2, which entails 3 consecutive rises in PSA levels at least 6 months apart. This definition has high specificity but low sensitivity. There are also important confounding factors, which include prostate-specific antigen (PSA) bounce (occurring in approximately 15% of patients) and expected PSA rise after stopping androgen deprivation therapy (ADT).
Recurrence after radical prostatectomy can be either local or systemic. In systemic recurrence there are several unique features:
- Rapid PSA doubling time (PSADT) of less than 3 months – occurs in approximately 10% of patients
- Positive metastatic evaluation
In contrast, in local recurrence the following features are present:
- Rising PSA confirmed on repeat evaluation
- Negative metastatic evaluation
- Positive prostate biopsy at least 18 months after radiotherapy
Local recurrence in the prostate following treatment with radiotherapy manifests with several immunohistological findings:
- Poorly formed and haphazardly arranged glands
- Nucleoli often inconspicuous
- Positive PSA staining
- Indolence
Dr. Eastham moved on to describe the patterns of local failure following radiotherapy in a large cohort of men treated at his center in Memorial Sloan Kettering Cancer Center (MSKCC)1. These 284 men with biochemical recurrence (BCR) had a post-irradiation biopsy. Their median PSA at failure was 9.9 ng/ml, with a median time to biopsy of 61 months. The post-treatment biopsy in these men showed cancer in 65% of patients, treatment effect in 31% and no findings in 4%. Only 4% of the patients demonstrated to have cancer in a new location, and Gleason upgrading occurred in 43% of patients.
The treatment options of such men with local recurrence after radiotherapy include:
- Observation with delayed use of ADT
- Immediate hormonal therapy
- Salvage therapeutic options:
- Radical prostatectomy
- Cryotherapy
- High intensity focused ultrasound (HIFU)
- Brachytherapy/HDR
The evaluation of such patients for potential local treatment should include answers to three important questions:
- Is cancer potentially curable with a salvage procedure?
- Is the patient appropriate for local salvage treatment? (acceptable life expectancy, motivated patient, and willing to accept the risks of such treatment)
- Would the treatment be safe?
The EAU guidelines list the following criteria for selecting men for salvage radical prostatectomy:
- Clinical stage T2b or lower
- Preoperative PSA less than 10 ng/ml
- Post -radiation biopsy Gleason score of 7 or less
The option of salvage radical prostatectomy is not widely accepted due to doubts about long term oncologic efficacy and a historically high peri-operative morbidity. The oncologic results demonstrate a 5-year progression free-probability of 54% after salvage radical prostatectomy (Figure 1):
Figure 1 – Progression-free probability of salvage radical prostatectomy
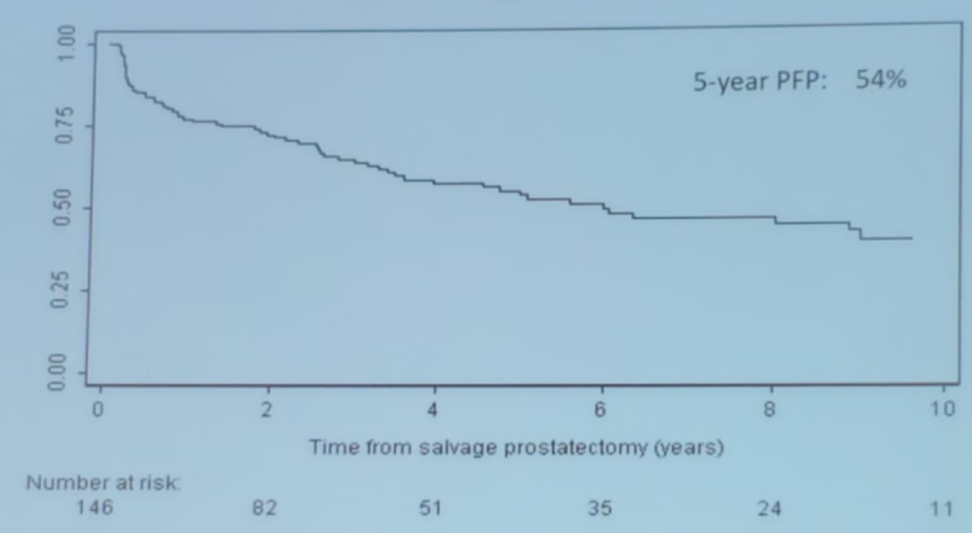
In a series of 124 patients who underwent salvage radical prostatectomy at MSKCC, 74 patients were free of BCR and 49 patients had BCR. Only 1 patient experienced clinical local recurrence2. There is also a large multicenter series of patients who underwent salvage radical prostatectomy (404 men) from 1985-20093 which Dr. Eastham mentioned. In this series, the median age at salvage radical prostatectomy was 65 years, with a median PSA of 4.5 ng/ml. Following the salvage procedure, 195 patients experienced BCR, 64 developed metastases, and 40 died of prostate cancer. At 10 years after salvage radical prostatectomy 37% (95% CI 31-43%) were BCR-free, 77% (95% CI 71-82%) were metastasis-free, and the prostate cancer-specific survival was 83% (95% CI 76%-88%)3.
When assessing only the low-risk patients in this study (approximately 30% of the cohort), who had a pre-salvage PSA of less than 4 ng/ml and post-radiation biopsy Gleason score of 7 or less, the results were considerably more favorable. These groups of patients were 51%, and 95% BCR-free and metastasis-free, respectively, and their prostate cancer-specific survival was 100%.
In conclusion, the long-term progression-free probability of patients with BCR after radiotherapy undergoing salvage radical prostatectomy, by pathological stage, is comparable to standard radical prostatectomy. Salvage radical prostatectomy provides excellent local control with superb cancer-specific survival for appropriately selected patients.
Presented by: James Eastham, MD, FACS, Professor and Chief of the Urology Service, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York, New York
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New York, USA, Twitter: @GoldbergHanan at the 39th Congress of the Société Internationale d’Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:
1. Jalloh M, Leapman MS, Cowan JE, et al. Patterns of Local Failure following Radiation Therapy for Prostate Cancer. The Journal of urology 2015; 194(4): 977-82.
2. Paparel P, Cronin AM, Savage C, Scardino PT, Eastham JA. Oncologic Outcome and Patterns of Recurrence after Salvage Radical Prostatectomy. European Urology 2009; 55(2): 404-11.
3. Chade DC, Shariat SF, Cronin AM, et al. Salvage radical prostatectomy for radiation-recurrent prostate cancer: a multi-institutional collaboration. Eur Urol 2011; 60(2): 205-10.
