Las Vegas, Nevada (UroToday.com) Dr. Michael Sheetz presented on the regulatory and radiation safety requirements for radiopharmaceutical therapy. He began with some basic facts on the radiation regulatory oversight. This is being done by regulatory agencies:
- The nuclear regulatory commission (NRC)
- Agreement state
Radiopharmaceutical therapy is covered under 10 CFR 35.300 (use of unsealed byproduct material for which a written directive is required). Radiopharmaceuticals must have FDA approval, or covered under the investigational new drug (IND) protocol.
An “Authorized User” is the physician responsible for the administration of radioactive material to patients. The authorized user must meet the specific training and experience requirements. The training must be recent, being done within the last 7 years, and approved by the regulatory agency. There are several authorized user pathways. These include certification by NRC recognized medical specialty board (American Board of Nuclear Medicine, radiology or Osteopathic board of radiology).
The authorized user must have completed at least 700 hours of training and experience, including a minimum of 200 hours of classroom and laboratory training.
The “Written Directive” is defined as the documentation required before the administration of any therapeutic dosage of unsealed byproduct material. The written directive must contain the patient’s name, the name of the radioactive drug, dosage, and route of administration. It must be dated and signed by the authorized user. The procedure for administration requiring a written directive is as follows:
- Verification of patient identity
- Verifying administration is in accordance with the treatment plan and the written directive
- The written directive form provides a checklist of the required information
Next, Dr. Sheetz brought up the topic of dose determination. This requires direct measurement of radioactivity, decay correction-based on the activity determined by the manufacturer. The administered dosage to patients must be within +/- 20% of the prescribed dosage.
Patient release criteria are an important issue that needs to be clear. The patient release criteria allow the release from hospital control of any patient who has been administered radioactive material if the total radiation dose to any other individual from exposure to the released patient is not likely to exceed 5 mSv (500 mrem). After treatment, the patient must be given written instructions to maintain radiation doses base on the principle of “as low as reasonably achievable” (ALARA) if the exposure to any other individual is likely to exceed 1 mSv (100 mrem). The 0.5 mSv limit to an individual is for each patient treatment, not an annual limit. An example of standard instructions given to patients after receiving I-131 sodium-Iodide therapy is shown in Figure 1.
Figure 1 – Standard instructions for patients receiving I-131 Sodium Iodide therapy: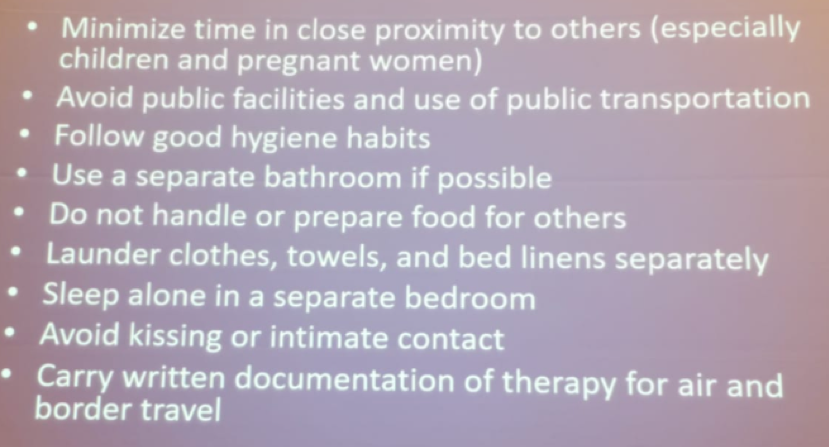
The next topic discussed was the considerations for radioisotope therapy infusion suite, where the treatment takes place. These include the dimensions of the room, the required presence of the adjoining bathroom, absorbent padding, being close to “hot lab”, and having a nursing support station. Moreover, the infusion room needs to be radiation-shielded with the minimum required distance from other facilities, consisting of lead line walls and a shielded patient cubicle.
Emergency contingency plans need to be created for the appropriate situations – such as spills, plumbing issues during administration, emergent patient medical emergencies and standardized algorithms for situations when patients need to be admitted.
Radioactive waste disposal is critical as well. It is acceptable to allow decay in the storage of radionuclides that have half-lives of less than 120 days. It is typical to hold these radionuclides for at least 10 half-lives, after which it is permissible to regularly dispose of the radionuclides when the radiation levels emanating from them are indistinguishable from their background.
Concluding his important talk, Dr. Sheetz emphasized the need to know the regulatory requirements and radioactive materials license conditions for the therapeutic use of radiopharmaceuticals. Most importantly, patient education, understanding, and cooperation are key for treatment success.
Presented by: Michael Sheetz, MS, CHP, DABMP, clinical assistant professor of radiology in the University of Pittsburgh’s School of Medicine, has been appointed to the U.S. Nuclear Regulatory Commission’s (NRC) Advisory Committee
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New-York, USA @GoldbergHanan at the 2019 SNMMI Therapeutics Conference: Therapies, Theranostics, and Building Your Radionuclide Clinical Practice, October 25-27, 2019 in Las Vegas, Nevada.
